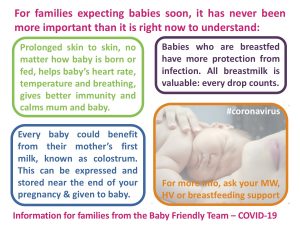
COVID-19 Infant Feeding Update – March 2020
Infant feeding leads and peer support co ordinators from across the Lancashire and South Cumbria area have brought this information together in March 2020 to support good decision making during the COVID-19 crisis.
We have provided information for formula feeding and breastfeeding support on separate pages, but of course it may be that as a family you need to access both.
Information on how to assess baby’s feeding and growth without access to weighing at Well Baby clinics, is also provided.
It has been agreed across Lancashire & South Cumbria that what have been known as ‘breastfeeding peer supporters’ will be offering support and information to ALL families about all things infant feeding in the immediate future, not only breastfeeding families requiring breastfeeding information.
There’s also a graphic for those who are expecting baby soon:

Why isn’t powdered formula milk sterile?
Alison Sauer, LIFIB member Unlike ready to use liquid formula milk, powdered formula is never sterile. This is because of the way it is produced. Firstly, this is a food, not an intravenous medicine. Food production conditions are not sterile. They limit the number of microbes and contaminants allowed in the product rather than prohibit them. This means microbe levels…

The truth about breastfeeding and risk
In recent weeks there has been media attention given to the somewhat distorted version of a sad story of a family in The United States of America whose baby was born in hospital and unfortunately died three weeks later from complications. These complication are thought to have resulted from insufficient feeding. This was a particularly complicated medical case and there were clear markers in the story for those who know about infant feeding and infant health, that all was not well from the very beginning, however it seems the mother was not made aware of the warning signs for insufficient milk transfer and that the markers were overlooked by those medical professionals involved in the family’s care who might have been able to intervene.
However, this LIFIB piece does not look at the single tragic story of a family’s loss, but instead at the possibly thousands of new families who have seen this press attention and the half-stories which have been published, and become frightened into believing that breastfed babies cannot thrive on breastmilk alone.
LIFIB’s job is to pull together the experience and evidence base around all things infant feeding, and to present it to you. We share here a couple of pieces from elsewhere on the internet which might help to allay your fears if you are one such family:
First of all, from Snopes.com, described as “the definitive Internet reference source for urban legends, folklore, myths, rumors, and misinformation.”
“Can Breastfeeding an Infant Have Deadly Consequences?”
And from the Unicef UK Baby Friendly hospital Initiative:
“Hypernatremic dehydration: Response to news coverage”
If you have a look around the internet it’s likely there will be other reports and articles too.
Meanwhile, the dangers of formula feeding are well documented, and even sometimes reported in the press – see this sad sad story of a baby who died just last year in the USA, and the warning from the US government, here.
And more frequently, babies who are not exclusively breastfed have other harms from the infant formula such as allergy and increased disease – here’s a report from this week.
It comes down to this: breastfeeding has been the way we have fed our babies since humans were mammals – and any deviation from the biological norm whether it is instrumental birth, blood transfusion, smoking, drinking or taking medications, eating lots of processed food stuffs. being overweight or not getting exercise, and indeed not breastfeeding, will come with the risk of potential harms of that deviation from the norm. So while many of us may know a story of someone who smoked 40 a day into their 90’s, really no one in 2017 would dream of saying that smoking was not bad for health.
Some of the risks of deviation from our biological norm, from feeding artificial milk, can be mitigated by behaviour such as using sterile liquid feed, within an appropriate time of manufacture to ensure the nutrients are still in the correct levels within the product, making up powdered formula milk correctly, learning to bottle feed in as responsive a way as possible for the baby, or if mum is breastfeeding then keeping levels of undesirable things which may pass into milk that mother is eating or drinking, down to a minimum, and so on – and all will affect different individuals in different ways – but the risks of deviations from the biological norm, remain.
Not feeding a baby is against the biological norm. Many birthing practices are against the biological norm, and artificial feeding is against the biological norm.
CPHVA conference this coming week – WHY the industry funding and bias, still?
Here is the line up for the 2016 CPHVA conference, taking place on 15th and 16th November in Telford. Here are some pictures of the layout in their magazine ‘Community Practitioner’, received by a LIFIB member recently. Just have a look at the ‘supported by’ organisations for a large proportion of the talks: Colief for the colic talk, Bio-Oil for…
Stop Press! Milk Matters is available as 2 inexpensive e-books!
You may have read our earlier piece about the life-work of Maureen Minchin ‘Milk Matters’ published in 2015 and which she toured the UK to speak about earlier in 2016.
“This book is a revelation”, said one reader. The revelations are solidly based on decades of research and working with families of allergic children. In fact, there are three inter-related books within this one large hardback.
Book 1 argues the Milk Hypothesis, that immune damage has been acquired vertically, compounding intergenerationally, through early infant nutrition; and that infant nutrition is the single most important contributor to the diseases of ‘modern’ societies;
Book 2 documents the ongoing real life experiment of infant formulas, and their known and emerging consequences for lifelong health. It reveals frightening facts from industry-funded research, and explodes the pervasive myth that industrial products are “nearly as good” as breastmilk;
Book 3 links the science and history to everyday infant problems, like colic, reflux, disturbed sleep and allergy of every kind, giving practical advice about current controversies, and preventing or resolving such diet-related distress in young children.
Those who read this book will be convinced of the necessity of enabling women to breastfeed their children, and the urgent need to provide women’s milk for children whose mothers cannot do so.
If enough people read it, western society will have to change; and both current and future generations will suffer substantially less unnecessary illness and early death.
And the WONDERFUL news is that the three books within the hardback Milk Matters are now available as 2 inexpensive e-books for everyone to access.
Kindle UK£7.70 each
Kobo CAN$10.09 each (about £6.01 – correct on Nov 5th 2016)
iTunes US$9.99 each (about £7.98 – correct on 5th Nov 2016)
Green contains books 1&2, which is the science and history; purple contains book 3, which is the practical allergy guide most appropriate for families.
To get a taster of what is within the 831 pages, thanks to Iona Macnab of iLactation you can get the big picture of what Maureen is saying in her book ‘Milk Matters: infant feeding and immune disorder’ by watching a presentation she did for them in 2015. We urge you to take the time out to watch this, because it will serve as a guide to what you need to know and can find out in the fully referenced book, which takes many many hours to get through. Click on the link to see all the slides and hear the talk. http://www.ilactation.com/present
Some reviews of the entire 3 book volume Milk Matters, are here:
“A life-changing book you need to read!”
Professor Mary Renfrew FRSE, Director, Mother and Infant Research Unit; Deputy Dean: Research, University of Dundee; Director, Scottish Improvement Science Collaborating Centre
“It’s a work of huge vision, based in extensive knowledge and understanding, yet it is easy to read and understand without specialist technical knowledge… A book to change the world, and people’s understanding of it.”
James Akré, WHO Nutrition (1980-2004)
“This is an important book, as relevant to gastroenterologists and genomic researchers as it is to unhappy parents of distressed babies.”
Katherine A. Dettwyler, Ph.D. Anthropology professor at the University of Delaware; author, Breastfeeding: biocultural perspectives
“Maureen Minchin has brought together a wide-ranging and extensive set of resources that will give readers a deeper understanding of how imperfect and problematic infant formula still is today. And she reminds us, once again, that breastfeeding truly matters. An incomparable gift to the world.”
Anthony F. Williams, Formerly Consultant in Neonatal Paediatrics and Reader in Child Nutrition, St George’s, University of London
“Minchin’s “milk hypothesis” uniquely brings together a lifetime of learning and practical experience. As she correctly observes, “There are many forms of evidence other than the scientific” so testing the hypothesis will require the cooperation of many conventional disciplines. It is to be hoped all those involved with infant feeding, whether as politicians, scientists, health professionals or parents, will give it serious consideration. Reading this book will no doubt be the starting point for fascinating research, but above all should stimulate greater global commitment to protect, promote and support human lactation and breastfeeding. Milk clearly does matter; the question is, just how much?“
Scary Mommy? Scary indeed…
Another instance of Similac targetting mothers with emotional trickery has risen up and is being shared on Facebook groups throughout the land. LIFIB are loathe to link to the piece but if you really want to read it, it’s here. Entitled “8 Thoughts That go Through A Mom’s Head During A Night Feeding” it is an attempt to build the ‘all…
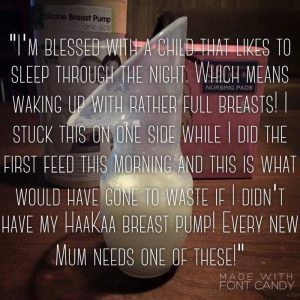
One-piece Silicone Breastpumps
By Shel Banks, Chair of LIFIB, Infant Feeding Information Specialist and IBCLC
An earlier version of this piece was first published on the blog for Growing Families ahead of their conference in Manchester in October 2016. This current piece has been amended and updated as new information has been made available, and to the best of our abilities we will continue to amend and update where new evidence is produced which materially changes the content.
This year’s big thing in the infant feeding related products world seems to be the Haakaa silicone breast pump. Coming from New Zealand, the company information on Facebook says they are a “baby brand that provides parents with Safe, Natural, Non-toxic, Eco-friendly baby products” http://www.haakaa.co.nz/ The ‘buzz’ around this product is so strong that people all over the UK have been importing from the other side of the world so they can get their hands on this item, and leaving rave reviews! I have been hearing a lot about them and wanted to provide a good discussion of what the fuss is all about.
This new-ish product is essentially a clever combination of two items which have been around for a long long time – breast shells and breast relievers.
Breast shells are designed to be tucked into the bra of a lactating woman, and the hole goes around the nipple so that any leaked milk is caught in the ‘shell’. The shape of the part which touches the breast, and the size and placing of the hole, creates gentle pressure on the lactiferous ducts behind the areola and actually encourages milk flow and so stimulates leakage.
Breast relievers are designed to pump milk from the engorged breasts of lactating women when the baby they have been feeding baby cannot or does not wish to be fed. They rely upon a combination of suction (creating a vacuum which draws the milk out), rhythm (which might stimulate the ‘let-down’ reflex) and pressure on the lactiferous ducts, which stimulates milk flow. These devices have been around for well over 100 years and are still used today. See this one  in the British Science Museum which was apparently in production between 1870 and 1901, although many like this were used much more recently – but also this one which is one of many similar ones available online now.
in the British Science Museum which was apparently in production between 1870 and 1901, although many like this were used much more recently – but also this one which is one of many similar ones available online now. 
Where these have been promoted as breast ‘pumps’ in the past I have been a little concerned as this suggests the milk is being saved for use in feeding baby, and I’m never sure how one would effectively clean the ‘bulb’ – which both gets squeezed to create the vacuum / pumping, and also serves to store the collected milk. Nor whether the plastics or rubberised materials used, might leech substances into the milk – which is a worry if this is to be used for feeding baby, but of less concern of course if it is purely used to relieve engorgement and the resulting milk is discarded. However I don’t know many lactating women who are happy about the idea of discarding breastmilk!!
So when I first saw the Haakaa in a breastfeeding group online I was impressed by the simplicity of the design and the ethos behind it – namely that it’s simple to care for, and non-toxic!
How does it work?
For this we can turn to the company’s own website: “Simply suction to your breast and let the pump do the work for you as it draws your milk using suction”. It’s true – the reports I have had tell me that the flange is placed on the breast, nipple lined up with the ‘neck’ of the device, and then the bulb is squeezed to compress which expels air from the bulb and creates a vacuum around the flange on the breast, securing it to the breast. Mums tell me that they then feed their baby on the other breast and while they are feeding the device fills up with their milk! The device has a scale on the side up to 90ml but I suspect it would accommodate 100ml – whether it could do this without falling off the breast as the vacuum reduces and the device itself becomes heavier with milk, is another matter – but you could hold it on.
How is it different from other pumps?
Most breast pumps work in a similar way – there’s a flange or funnel which sits on the breast, a hole and tube which accommodates the nipple, and then something on the other side to provide the vacuum in a rhythm so that it does actually pump the breast. Usually there’s some sort of valve so that the milk once removed from the breast is released into a bottle via some sort of ‘one way’ affair and cannot come back out again into the body of the pump. Whether hand pump or electric, whether double or single, costing £10 or £200 – all the same basic design. So there are at least 4 parts, of which at least 2 are moving. Usually many more than 4, and first time assembly for the exhausted new parent is akin to completing a passport application using only your mouth to hold the pen! But the Haakaa is just one piece of silicone and not really a ‘pump’ at all – no valve, no pumping required – though the manufacturers do say that you COULD squeeze and release the ‘bulb’ at the bottom, which contains any milk, if you choose to – it isn’t necessary. Because it involves no ‘pumping’, in spite of the dictionary definition of pump only meaning to move liquid through suction or pressure, for some reason I’m a little uncomfortable calling it a ‘pump’ and am finding myself using the word ‘device’ to describe it!
How can it be cleaned?
Unlike any of the more complicated ‘moving part’ pumps there’s only one piece to this device which makes it far simpler to wash inside and out (in hot soapy water) and of course no assembly required. Unlike its predecessors the breast reliever, Haakaa’s device is also dishwasher safe (not sure how to position it so that it would definitely get washed and rinsed thoroughly, however – dishwashers tend to send small light things like this spinning around inside the machine during the cycle, in my experience), and because we don’t want any nasty things leeching into baby’s milk they are made from 100% food grade silicone and certified BPA, PVC and Phthalate free. So it’s as simple as it looks.
Which brings us to a troubling issue with these devices:
Copycat pumps.
Since these devices have become popular, almost inevitably some copycat devices have spring up on the internet – some in China, some in Malaysia. Examples here
Some look identical to the Haakaa, some do not, and are not. The authentic Haakaa pumps were originally available only from New Zealand, costing $27NZ (about £15) and it was not possible to buy them from the UK without relatively high transport costs. The main (New Zealand-based) websites selling them would charge around £27 to sell and deliver one to an address in the UK, within about 2 weeks. UPDATE: at the bottom of this piece we have included a link for purchasing in the UK, updated 28th August.
However, the copycat pumps are available through amazon and other mainstream retailers, claiming prices from as little as £3 delivered! From the families I have spoken with who have ordered these copycat pumps, I know that the very cheap ones often do not turn up at all, and sometimes the refunds have been impossible to secure, also that even the £12-20 ones have been arriving without proper packaging – this is one example given to me by a local mum
As you can see – the packaging isn’t quite as sophisticated!
These copycat pumps are often more ‘solid’ than the authentic Haakaa, made from a material that feels more rigid to the touch, and weighs more – 100g compared to 74g. This suggests they are not made to the same standards as the authentic Haakaa. Reviews on some of the copycat pumps on eg Amazon.com suggest that this thicker silicone actually causes pain when it is suctioned onto the breast, and there have been reports of burns to the skin, like chemical burns, from users – the reviews on some of the third party selling sites containing these damning claims have now been removed as far as I can see.
Interestingly the copycat pump shown above donated by a local mum has a different pattern on the silicone to the Haakaa, but the design is identical and it’s just as squishy – even came shrink- wrapped squished in the post as you can see above! BUT it weighs LESS than the authentic Haakaa – so the copies are getting more sophisticated but still are not the real thing. The copycat pumps sometimes have Chinese lettering on them, whereas the authentic Haakaa one, a representative from the company tells me, have the word HAAKAA written down the side.
The authentic Haakaa pumps are certified BPA free. BPA is Bisphenol A – an industrial chemical used in the production of polycarbonate which is a hard, clear plastic, used in many consumer products. BPA is also found in epoxy resins, used as a protective lining on the inside of some metal-based food and beverage cans. It also leeches into liquids and is now thought to be carcinogenic, to which end it has been banned from the production of baby bottles since 2011 in the EU.
Buyer Beware!
Copycat pumps make some claims on the advertising and packaging but we cannot of course be sure if these are true. One mother I spoke to was concerned about these copycat pumps and, fearful she had bought one, she emailed the seller to ask if they were safe and what testing they had had. The response she received was that they had no idea, they were just selling and sending them out. In the UK/EU the importer actually has the responsibility for the safety and conformity of imported products, the ‘CE markings’, so if a UK resident is importing things from abroad then as the importer, THEY are responsible for checking that the products are appropriately CE marked for conformity to required standards.
Are they any good?
Assuming we’re now talking only about the authentic Haakaa silicone pump, what most families will want to know, I imagine, is are they any good?
If you go online and search for Haakaa reviews, a few clicks will bring you many many positive stories, lots of five star feedback, youtube videos and so on. The point is it’s a simple idea, and it works. Gentle pressure on the lactiferous ducts, plus gentle vacuum as the bottle expands, plus feeding baby or active pump on the other breast to create a ‘let-down’, will elicit a flow of milk into the device. Some women find they could completely fill it, others just an ounce – but as many mothers have told me – they have always failed at expressing, they are no good at it, and this device gives them an ounce they would never otherwise have had! Mothers who have trouble with leakage while feeding on the other breast and so use lots of breast pads, are finding this saves them lots of breast pads and leakage AND gets them some milk to store.
A word of caution though – a quick search of reviews online shows that some babies think it’s a great game to knock them off the other breast as they are feeding, and because of the design, a knocked Haakaa pump can spill ALL the milk collected – up to 4 ounces – all over the place. So now you have been warned about that, there’s no use crying…!
Lots of rave reviews however, and little images sent in of milk collected in them!
Are there any drawbacks?
However because they apply the gentle pressure on the lactiferous ducts AND a gentle suction too, they will encourage continued leaking and can exacerbate the issue for anyone for whom leaking is already an issue; so as breasts are really supposed to work individually – assuming you are feeding only one baby! – if you have a problem with leaking from one side when the other is ‘working’, or perhaps a slightly different but related issue such as an over-supply, perhaps it’s better to manage that rather than encourage more of the same by collecting the milk in a device like this. See someone qualified and experienced in supporting mothers with breastfeeding issues – perhaps from the voluntary sector (ABM, BfN, LLL or NCT) or an IBCLC www.LCGB.org/Find-An-IBCLC has a list of local practitioners.
Nutritional content of milk collected
One final potential drawback of these devices which should be noted before going ahead and using or encouraging their use, is that used as described above, ie simply attached to the breast and left to gather milk which is spontaneously ejected from the ‘other’ breast while feeding or expressing on the first breast, they may basically collect ‘drip milk’ which is not suitable for use exclusively as a full feed for baby, as it’s the watery carbohydrate-rich milk, not the fattier richer milk. Fat soluble nutrients will be contained in the fattier richer milk in greater quantities. Babies feeding directly at the breast of course access the full spectrum of milk which the breast is capable of making, via a combination of variations in pressure, suction and mum’s letdown.
If milk collected by the Haakaa or any other collection device is used as an occasional drink to be left when mum isn’t able to feed, then probably the only negative issue would be baby being slightly less satisfied or needing slightly more volume to become satisfied – not a big deal. However if you fed nothing but ‘drip milk’ to a baby it would not do so well. In milk banking ‘drip milk’ is not suitable for donation because it is not whole milk, essentially it’s skimmed milk.
A very quick search for evidence to corroborate my assertion about ‘drip milk’ when chatting online about the potential drawbacks of this device, brought me this from 1978 http://www.ncbi.nlm.nih.gov/pubmed/571325 – the author of that piece Alan Lucas does take money from the infant formula industry (though this was long ago so not sure whether this pre-dates the industry money) and so some may pooh-pooh the impartiality of his work, but we cannot dismiss everything he does on that basis alone – he has come up with some interesting stuff! And industry-funded work is often extremely informative too – no sense throwing the baby out with the bath water so to speak!
I know too from my experience working withthe UK Association for Milk Banking UKAMB for these past many years, and as a member of the 2009/2010 Development Group for NICE Guidance on Milk Banking, that the donation or collection of ‘drip milk’ is not recommended within milk banking as it is not suitable for fully-feeding growing vulnerable babies in the NNU, because of the nutritional shortfalls it may have. However, as an antidote, of course one could hand express a little of the much fattier richer milk from the breast after a feed, to even up the nutritional composition, and make it more suitable for using as a full milk feed. The best ‘how to’ guide I have seen online for massage before pumping and for expressing by hand is to be found here.
Because of the vacuum, it’s likely to be slightly less ‘drip milk’ than milk which is REALLY dripping out, but not much more than the milk elicited by the breast shells which apply pressure to the areola. In some of the photos posted online, the colour of the milk is suggestive of higher water / carbohydrate content and lower fat content – but of course composition of breast milk will be slightly different from mum to mum and from one session to another, and it’s impossible to judge nutritional content from a photo posted online! Haakaa confirm that there are no studies to determine the nutritional quality of the milk elicited as yet, and as a non-clinical researcher I’m certainly not in a position to provide this evidence myself.
It’s worth pointing out too, that though Haakaa’s website says “simply suction to your breast and let the pump do the work for you as it draws your milk using suction”, apparently the instructions inside the box that comes with the genuine Haakaa also state that milk can be elicited by ‘pumping’ the bulb of the device.
Other online blogs about this product
Most of the blogs I found – a quick google search brings up loads! – seem to be rave reviews about the product, or akin to an instruction manuals, rather than a look at how they work and why it’s so important to get an authentic one and not a copycat: however in this FB post from May, Ellen from New Zealand, who is a midwife, compares the ‘China Cheapie’ to the authentic Haakaa pump, and shows that they cheaper one is less flexible and much heavier.
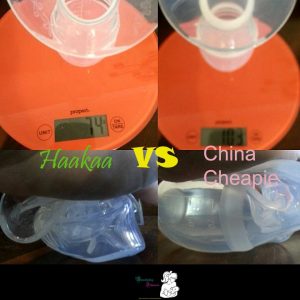
Taken from Breastfeeding Illawarra’s post about the Haakaa and the ‘China Cheapie’!
As reported above however, newer copycat pumps are now on the market which look much more like the authentic pump, and behave in a similar manner – the pattern on the pump is different on the one I have (authentic Haakaas have a bamboo pattern – this one is flowers!), but the shape, feel and function are almost identical. The main factors pointing to a copycat pump rather than an authentic Haakaa device are the packaging – this one arrived in the shrink-wrap shown earlier, and stuffed into a plastic mailing envelope, not the cardboard tube of the Haakaa pump – and the weight is just 5g less. So we have no idea what it is made from or where it was made.

As with everything, Buyer Beware – and in this case, you definitely get what you pay for – so if the Haakaa is the pump for you then be sure you order a genuine Haakaa!
One final note – I have, at time of writing, not seen a genuine Haakaa pump – and I have not trialed it as I am an IBCLC and researcher, not a lactating mother anymore, so this is all theoretical and historically based and gathered from currently available evidence. I would welcome new evidence or experience on anything related with which to update this piece.
Haakaa have updated me that the pump is now available direct in the UK, via Amazon at £16.10 including delivery via Amazon Prime – and since I have heard that people importing from overseas have been billed for import duty in some cases, this seems like the best way to buy now!
AUGUST 2016
.
How The Baby Friendly Initiative Supports Feeding of ALL Babies
I have just come across an article I absolutely do not agree with. I won’t link to it as the website promotes the sale of a book I suspect is as dreadful as the article, and I have no wish to promote it further: but I SHALL cut n paste here and then reply below.
(Shel)
“When the ‘Baby-Friendly Initiative’ is not baby-friendly at all”
“In Britain a quarter of all babies will never have breastmilk touch their lips. By the time a British baby is two months old, she is more likely than not to be exclusively formula-fed. Yet there is a conspiracy of silence around formula feeding, that means most of the mothers of these babies will never receive critical information from the people they trust – nurses, midwives and health visitors, about how best to bottle-feed.
“They’re not taught by a trusted health professional the best bottle-feeding position to reduce the chance of ear infection, nor are they encouraged to bottle-feed skin-to-skin to promote bonding, nor are they told it’s important they throw away all unfinished bottles after an hour.
“For the most part, they get basic information on how to make up a bottle from the side of a tin, and pick up other tips through crowdsourcing on the internet. Because those are really great ways to learn about one of the most important things you’ll be doing for your baby in the first few months of her life.
“This state of affairs is shameful, and negligent, and a large part of the blame must go to Unicef and its Baby-Friendly Initiative.
“The Baby-Friendly Initiative is Unicef’s hospital breastfeeding program. Its aim is to make hospitals more breastfeeding-friendly places – an admirable goal. It does this by giving accreditation to hospitals and other health services which implement its policies. At the moment, around half of the UK’s maternity services and health visiting services are certified ‘Baby-Friendly’.
“Unfortunately, this well-intentioned effort to make institutions more breastfeeding friendly has led to bottle-feeding mothers being ignored, their babies missing out on crucial health information, and promoted feelings of guilt and inadequacy because of its ‘breastfeed at all costs’ mentality.
“Last year the BFI changed some of its guidelines to supposedly better support bottle-feeding parents.
“This week, the lip-service nature of this change has been on full display at the University of Bradford.
“The story goes back a couple of months when myself and my co-author of Guilt-Free Bottle-Feeding, Dr Sasha Howard, were invited to take part in a debate about bottle-feeding by the University of Bradford’s Midwifery Society.
“Fantastic! We were over the moon. Student midwives who actually want to learn more about how they can help the 25% of mothers who will never breastfeed in hospital!
“This was a bigger deal than you might think – education about bottle-feeding in university midwifery courses is patchy or non-existent (a result of that ole’ conspiracy of silence again), leaving newly-minted midwives largely ignorant about formula and formula-feeding.
“So, Sasha and the lovely student representative were going back and forth about logistics, when suddenly, she received this email:
“Unfortunately we have had to put the debate on hold as the university won’t support the event. This is due to the university going through accreditation for BFI and being unable to show support for anything to do with artificial feeding.”
“Yes, you read that right – in order to gain ‘baby-friendly’ accreditation, simply talking about the way the majority of British babies is fed is taboo.
“It beggars belief and logic, and I would suggest the ethics of a caring profession.
“Any mother bottle-feeding mother who has felt let down by health professionals (and that’s most of them) should feel angry that Unicef’s BFI is encouraging a deliberate denial of information to young health professionals who want that knowledge, because they know they are going to need it in order to give the best care they can, to the most women they can.
“How is it baby-friendly to leave mothers with little to no knowledge about how they will, more likely than not, be feeding their baby in two months time? This ‘promotion’ of breastfeeding through denying the very existence of formula has to stop. It’s not ‘baby-friendly’, it hurts babies and their mothers.
“And the crazy thing is, the BFI doesn’t even really make that much of a difference to long-term breastfeeding rates. It has increased the initial uptake of breastfeeding, but a large study of low income British mums found women who gave birth at a BFI-accreditated hospital were no more likely to be breastfeeding at one month than women who had given birth in an unaccredited hospital.
“In Australia, there are far fewer BFI-accredited hospitals, but more women breastfeed, and for longer. There are many cultural reasons for this, but it shows that the big stick of the BFI is not the answer to improving breastfeeding rates.
“If the Baby-Friendly Initiative were really baby-friendly, it would recognise that the best thing it can do is support all babies’ mothers, regardless of how they feed their babies. The conspiracy of silence around formula, and the risk that lack of information creates to babies’ health, has to stop”
So, Baby Friendly aren’t very Baby Friendly?
And Baby Friendly facilities cannot talk about artificial feeding or bottles?
Do you know in the 7 years I have been the co-ordinator for the project around the Baby Friendly Initiative in a maternity setting in the NW of England, and in the few years before that when I worked on the BFI project in the community surrounding the hospital, so the 3 separate accrediations and 3 subsequent re-accrediations I have been involved in, no one from Unicef BFI has EVER told me that discussion of artifical feeding or bottles was prohibited: indeed, some years ago the fore-runner of LIFIB was evaluated by a university for Unicef BFI and the Dept Health to work out the value of it – a resounding success was declared, other areas wanted to join, and LIFIB was born.
Here’s the article if you are interested. http://www.ncbi.nlm.nih.gov/pubmed/22019088
Indeed, in my role as Infant Feeding Information specialist / Chair of LIFIB I am called upon to train health care professionals about various aspects of formula feeding including cows milk protein allergy, colic and reflux, lactose intolerance, paced feeding, responsive feeding, safer preparation of infant milks, etc. This is so that health professionals – in all of my area and in areas locally in the NW of England where I have worked, at least – can talk in an evidence-based way about infant formula, and bottles!
One of the standards assessed for community accreditation is around safer prep of formula for mothers who are not breastfeeding or not exclusively breastfeeding – and conversations with staff to support these informed choices and safer practices is encouraged.
In the many years I have worked in infant feeding and within the structure of BFI accreditation, I have only EVER heard the suggestion that BFI means that staff cannot talk about formula, in one place – at a formula industry-sponsored event outlined here https://lifib.org.uk/jfhc-sma-event-london-nov-2014
Last year at the Unicef BFI conference, Dr Helen Crawley the Chair of First Steps Nutrition, who specialise in providing evidence based information about infant formulas, was invited to speak and spoke for an hour on the subject. No one at Unicef BFI is stifling evidence based information about infant formula in my experience.
I wonder whether the Uni of Bradford, cited in the ‘article’ reproduced above, got wind of the fact that the speaker they had initially engaged may not be evidence-based and impartial, and rescinded their offer on that basis in fact?
Something to think about.
JUNE 2016
UPDATE August 2016: I have now read the book – bought online for 15 pence – and it’s as biased as I expected.
.
Maureen Minchin: Milk Matters
Those of our readers who have been involved in breastfeeding support for many years, will no doubt remember Maureen’s earlier books “Breastfeeding Matters” and “Food For Thought” – virtually mandatory for all breastfeeding counsellors in the 1980s and 1990s. Since then, whilst some subsequent editions of those two valued texts have been published, Maureen has gone to ground, working on her milk hypothesis, supporting families in need of information about their infants, and gathering evidence: from that has come the new “Milk Matters” – a three-in-one book for parents, GPs, peer supporters, nurses midwives and health visitors, paediatricians dieticians and researchers alike.
Maureen visited the UK in April, May and June 2016 to speak on various themes of the book and made herself available to us all at workshops and study events from Basingstoke to Edinburgh to Skipton to Manchester to Leicester and London – and many more.
LIFIB were included in her tour, speaking about infant milks to a varied audience of breastfeeding peer supporters and health professionals at an event at Wallasey Town Hall on the Wirral on the 18th May, along with LIFIB representatives and Dr Helen Crawley from First Steps Nutrition.
LCGB – the Lactation Consultants of Great Britain – have the honour of hosting Maureen’s 4 parallel full day study events up and down the country – on breastfeeding the allergic infant, as well as having two appearances on different subjects, at their annual conference in Basingstoke on the 15th and 16th April.
Maureen spoke at the LLL Spring Workshop in Skipton in late April, and finally an appearance at The Breastfeeding Festival in Salford, 25th and 26th June and talks to peer supporters, midwives, health visitors and Consultant Paediatricians in Blackpool on 1st July concluded Maureen’s visit to the UK. These talks will all cover different aspects of the the book and Maureen’s experience and expertise gathered across decades.
Here are some reviews:
“A life-changing book you need to read!”
Professor Mary Renfrew FRSE, Director, Mother and Infant Research Unit; Deputy Dean: Research, University of Dundee; Director, Scottish Improvement Science Collaborating Centre
“It’s a work of huge vision, based in extensive knowledge and understanding, yet it is easy to read and understand without specialist technical knowledge… A book to change the world, and people’s understanding of it.”
James Akré, WHO Nutrition (1980-2004)
“This is an important book, as relevant to gastroenterologists and genomic researchers as it is to unhappy parents of distressed babies.”
Katherine A. Dettwyler, Ph.D. Anthropology professor at the University of Delaware; author, Breastfeeding: biocultural perspectives
“Maureen Minchin has brought together a wide-ranging and extensive set of resources that will give readers a deeper understanding of how imperfect and problematic infant formula still is today. And she reminds us, once again, that breastfeeding truly matters. An incomparable gift to the world.”
Anthony F. Williams, Formerly Consultant in Neonatal Paediatrics and Reader in Child Nutrition, St George’s, University of London
“Minchin’s “milk hypothesis” uniquely brings together a lifetime of learning and practical experience. As she correctly observes, “There are many forms of evidence other than the scientific” so testing the hypothesis will require the cooperation of many conventional disciplines. It is to be hoped all those involved with infant feeding, whether as politicians, scientists, health professionals or parents, will give it serious consideration. Reading this book will no doubt be the starting point for fascinating research, but above all should stimulate greater global commitment to protect, promote and support human lactation and breastfeeding. Milk clearly does matter; the question is, just how much?”
The book is for sale online via Wordery for the lowest price for UK deliveries, and we at LIFIB thoroughly recommend it!
UPDATED to add that two out of three of the books within Milk Matters are now available as e-books – see update HERE.

Who is buying your loyalty with their study days?
News of some potentially enticing upcoming free study events for health professionals, heavily sponsored by and attended by infant milk manufacturers, in Manchester and Birmingham. Already many of our colleagues have been talking about these study events in forums online, and students from a number of the midwifery / health visiting courses in the NW have been circulating the information…